Radial artery catheter failure
2.5 million radial arterial catheters (RAC) are used annually in Europe (USA: 8 million), commonly to monitor arterial blood pressure and take blood samples in surgical, A&E and ICU units. They can fail. For a study of mechanisms that might lie behind premature RAC failure and complications related to RAC in clinical use*, at team at the Radiology/Ultrasound and Anaesthesiology Department, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, USA, used SonoScape’s S9 hand carry ultrasound system.


The clinical trial aimed to determine the causes of RAC failure and confirm whether a low artery diameter to catheter diameter ratio leads to decreased local blood flow and thrombosis. Using the S9 ultrasound system with a 12 MHz linear array probe to evaluate and monitor the RAC insertions as well as blood flow dynamics in the radial and ulnar arteries, the 25 enrolled patients were scanned before RAC insertion, immediately after, and intermittently every two to four hours during the day and every four to six hours during the night (for 24 to 36 hours). By using the S9 ultrasound, the researchers could literally see what was happening in the ulnar and radial arteries of the patients, Sonoscape reports.
‘Using the S9’s greyscale and Doppler technology, measurements were taken of blood flow and the diameters of both the ulnar and radial arteries. Assessments of RAC insertion factors also allowed for measurements for the composite vessel trauma score for respective arteries after insertion. To analyse the data, a paired Student t-test and a Wilcoxon Rank-Sum test were used to compare results.’
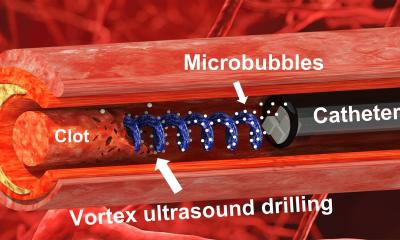
For the study, RAC initial failure and final failure were classified as difficulty/inability to aspirate blood through the RAC or a dampening/loss of the blood pressure waveform. 211 ultrasound scans were obtained from 25 patients. 21 had experienced a RAC initial failure; four experienced RAC final failure. ‘With the S9’s high image clarity, the reasons for RAC failure were easily revealed,’ SonoScape reports. ‘Each failed for a different reason: ranging from the catheter being outside the vessel and in the subcutaneous tissue, the RA catheter tip against the arterial wall, thrombus on the catheter tip partially/completely obstructed the RA catheter lumen, and thrombus within the RA lumen partially/completely obstructed RA blood flow.’
Soon after RA catheter insertion, the RA and UA inner diameters increased from 2.21±0.4 mm to 2.54±0.45 mm and from 1.91±0.44 mm to 2.23±0.48 mm respectively (no significant differences in RA and UA diameters), the study showed. For the 24 RACs that did not have a final failure, the median number of cannulation attempts was nine and the median CVTS was 8.5. Comparatively, the CVTS for the four RACS that developed a final failure was 8.3 and the mean number of blood draws was 5±3.3. Median time to initial dampening of the RA waveform was 5.9 hours in 22 cases.‘Using the S9’s colour Doppler the team could measure the velocities in the RA and UA arteries after RAC insertion. In the RA artery, the peak velocity decreased from 56.2±18.7 to 36.6 cm/s after the RAC was inserted. Peak velocity in the UA, however, increased from 53.7±19.3 to 63.4±20.5 cm/s after insertion of the RAC. Ultrasound scans also did not indicate a difference in vessel diameter or blood flow velocity when comparing successful RACs to that of the four that developed a final failure; however, this may be attributed to the limited number of final failures that were observed.’
There was also no difference in velocity patterns or in diameter in the RACs that failed compared to those that did not fail. A threefold conclusion. Both the RA and UA experienced significant dilation after RAC insertion. The data suggested that vasodilation and increased blood flow around the catheter might help to prevent thrombosis and protect the function of the arterial catheter. In some patients the peak blood flow velocity significantly decreased after insertion of a 20g catheter, especially in the RA with a small inner diameter.
With the S9’s high-resolution ultrasound imaging abilities, in vivo observations were possible to reveal what caused RAC failure during the patient’s clinical course. Failures consisted primarily of torturous vascular anatomy and RAC tip obstruction, thrombus formation on the RAC tip, and partial/complete thrombosis of the RA lumen.
* Study presented at the World Federation for Ultrasound in Medicine and Biology (WFUMB) Annual Convention and Preconvention Programme in October.
Source: SonoScape Medical Corporation
31.07.2015