Politics
New EU recommendations on Cytotoxic Drugs
New policy recommendations on preventing occupational exposure to cytotoxic drugs were launched in the European Parliament on 26 April 2016, an important new initiative designed to protect healthcare professionals working across the EU.
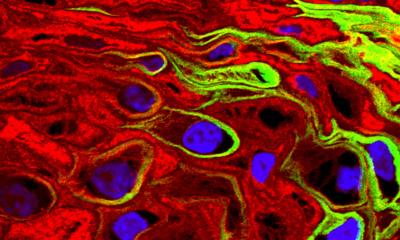
Cytotoxic drugs, primarily used to treat cancer, are classified as hazardous and can cause adverse health effects from exposures in the workplace. Unsafe handling of cytotoxic drugs has been reported to cause cancer, organ toxicity, fertility problems, genetic damage and birth defects. The more common routes of exposure are contact with skin or mucous membranes, inhalation and ingestion.
With incidents of cancer continuing to increase, the use of cytotoxics is also rising. Cytotoxic drugs are also now increasingly used to treat haematology and rheumatology, so both the number and range of healthcare professionals handling them is also on the rise, with nurses, pharmacists and pharmacy technicians at the highest risk of exposure.
Although the increasing risk has been recognised in Europe - by bodies such as the European Agency for Safety and Health at Work - there is no legislation, guidelines or minimum standards in place for EU member states on handling cytotoxic drugs. However, in November 2015, the European Parliament called on the Commission to take action on chemical risk factors, including exposure to hazardous drugs. The new recommendations paper, Preventing occupational exposure to cytotoxic and other hazardous drugs, calls for legislation to be put in place and also advises on best practice to prevent exposure.
Continuous education of healthcare providers, along with the use of appropriate personal protective and drug handling equipment are recommended as vital to effectively prevent exposure to hazardous drugs.
The recommendations paper highlights Closed System Transfer Devices as the only equipment that has been specifically designed to protect healthcare workers from occupational exposure to hazardous substances, but warns that ‘some equipment suppliers claim that their devices are closed even if they produce aerosols, vapours and dripping.’ As damage can be caused by inhaling cytotoxic drugs, the authors of the paper call for a common definition for ‘Closed-System Drug Transfer Devices’, detailing the technical specifications required to be met.
Dr. Paul J.M. Sessink, Exposure Control Sweden AB, who contributed to the recommendations, says: “With the use of cytotoxic drugs continuing to rise, we need to protect the healthcare professionals handling them from exposure and adverse effects. The health and wellbeing of healthcare workers is our primary concern, but preventing exposure will also contribute to the sustainability of European’s healthcare sector by increasing morale and preventing absenteeism of staff.”
Johan Vandenbroucke, Senior Pharmacist Production at Ghent University Hospital and another contributor to the guidelines adds: “Although the dangers of exposure to cytotoxic drugs have been well known for a number of years, there is no official guidance or legislation in place in Europe. Hopefully these recommendations will be the first step towards establishing EU-wide minimum standards.”
26.10.2016