Article • Fertility
Social freezing on demand in the future
Since 2006 around 100 centres that offer fertility preservation for cancer and non-cancer patients in Austria, Germany and Switzerland have joined forces to form the FertiPROTEKT network.
Report: Brigitte Dinkloh

This is affiliated with the FertiPROTEKT register, which documents the measures implemented to preserve fertility and the respective results achieved. Medical freezing, i.e. freezing of human germ cells or tissue, plays an important role in bringing the dream come true of having a baby at a later stage.
About two years ago, when Apple and Facebook in the USA promised their female employees to cover the costs of literally putting their desire to have children on ice, this also started a heated discussion against the pros and cons of ‘social freezing’ (meaning freezing one’s own eggs for insemination later in life) on this side of the Atlantic. Fact: Social freezing is now also possible in Europe, but the figures are a lot lower than for medical freezing. According to the register for Germany, Austria and Switzerland, there were 406 consultations for non-medical indications with 257 treatment cycles, with an average of 9.4 eggs per cycle being cryopreserved. This compares with 1,059 consultations carried out in 76 centres in the context of fertility protection for medical reasons, with 801 patients opting for treatment.
‘Medical freezing in Germany is carried out in the context of FertiPROTEKT, whilst social freezing is clearly more controversial,’ explains Professor Ludwig Kiesel MD, Director of the Department for Gynaecology and Obstetrics at Münster University Hospital and representative of the division of Reproductive Biology and Medicine at the German Society for Endocrinology, which held its 60th congress in Würzburg this March.
Indications for medical freezing

The most common indication for cryopreservation is breast cancer, followed by Hodgkin’s lymphoma, leukaemia, and other cancers. Benign diseases, such as rheumatism or Turner syndrome play a subordinate role. A new guideline, which Kiesel helped to develop, therefore recommends that all oncology patients up to the age of 35 should receive advice on options for fertility protection. Currently there are many more cases of disease compared to the number of consultations and measures implemented for fertility preservation. ‘The problem is that tumour treatment must often start at fairly short notice, and many colleagues literally forget to offer their patients advice. Egg harvesting can only be carried out once the patient has been receiving hormonal stimulation for two weeks, in the same way as is done in the context of assisted reproduction.
With cancer treatment imminent, there is little time and decisions must be made quickly. Most patients who do not yet have children, or only one child, express an interest in fertility preservation’, the gynaecologist explains. According to the new guidelines, all oncology centres will now have to offer advice on fertility preservation based on clearly defined standards. In Germany there are around 100 of these centres and, if a medical professional does not have the required competence, the guidelines ensure that the patient receives advice through a cooperation partner – a procedure already implemented at Münster University Hospital. ‘After all, cancer treatment is carried out in many medical fields and not just in gynaecology and urology,’ the professor points out.
Vitrification
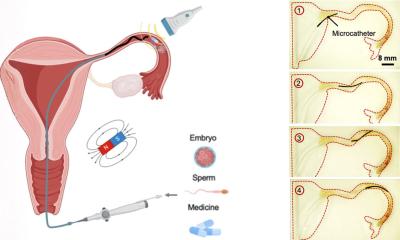
Cryopreservation provides the opportunity to harvest eggs as well as ovarian tissue, with around half the tissue from one ovary being removed at Münster University Hospital for this purpose. The tissue is flash frozen in the same way as fertilised or unfertilised eggs. Vitrification, i.e. flash freezing is particularly sensitive and durable procedure and better than its predecessors. Once the tumour has been treated successfully, and the patient would like to become pregnant, the cells or tissue can then be re-implanted.
‘The patient should either have been free of the disease for a certain period of time or should be very apt at managing it. The tissue is re-implanted where it was removed. This should enable the patient to become pregnant naturally,’ Kiesel explains. There are other measures for protecting the reproductive glands apart from cryopreservation. Medication can be administered, or the ovaries can be transposed. Even though these procedures may be more likely to attract funding from health insurers, Kiesel believes that cryopreservation is the safer method. However, whether or not the costs, of at least €2,500, will be reimbursed always depends on the individual case.
Chances of success
Be it social freezing or medical freezing, the younger a woman is at the point of harvesting/removal the higher the chances of success for a successful pregnancy will be. Kiesel: ‘This is not a law as such, but we generally recommend egg harvesting up until the age of 35. After that the quality of the cells becomes more unfavourable. However, particularly in the case of social freezing, many women above this age opt for the procedure, because they often only face up to the issue of family planning once they are caught between the priorities of continuing a successful career and the desire to start a family.’ Kiesel therefore believes that the trend towards fertility planning will become inevitable. ‘I foresee that these services will be offered to both women and men. And there will also be European employers who will offer it. As Carl Djerassi has predicted: Social freezing will become standard in the future.’
Profile:
Ludwig Kiesel MD PhD studied medicine at Ruprecht Karl University, Germany, and the Royal Free Hospital Medical School, London, UK. In 1981-82 he was a research fellow in Maryland, at the National Institutes of Health. After residency at Heidelberg University he joined Tübingen University and then chaired Obstetrics & Gynaecology at Münster University. Kiesel is also a board member of the World Endometriosis Society, German Society of Gynaecological Endocrinology and German Society of Obstetrics and Gynaecology.
24.04.2017