Image source: Adobe Stock/PRB_ARTS
News • Breakthrough against metastatic mammacarcinoma
New approach busts chemo resistance of TNBC breast cancer
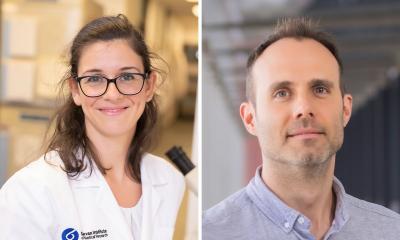
A team of researchers at the Medical University of Vienna has discovered that dormant tumor cells surviving chemotherapy can be targeted through the inhibition of a specific protein called P-glycoprotein (P-gp).
This discovery opens up new possibilities for delaying relapse and is particularly relevant for aggressive triple-negative breast cancer (TNBC), for which there are currently few effective treatments. The findings, published in the journal Drug Resistance Updates, could represent a step forward in the treatment of this type of cancer.
Triple-negative breast cancer is a particularly dangerous form of breast cancer. It is characterised by an early relapse and a poor survival rate. Until now, there have only been limited treatment options, and chemotherapy protocols are often not sufficiently effective. Therapy resistance, where cancer cells do not respond to conventional treatments, has long been a major problem. A research team at MedUni Vienna's Center for Cancer Research has now discovered why this happens and how it can be prevented.
The discovery that P-gp contributes to the removal of toxic lipids from rare surviving cancer cells represents a vulnerability that can be exploited to prevent relapse
Gergely Szakács
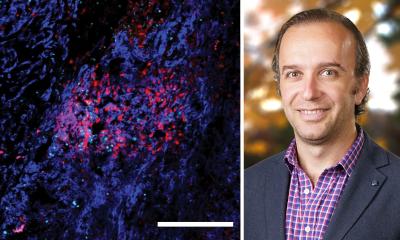
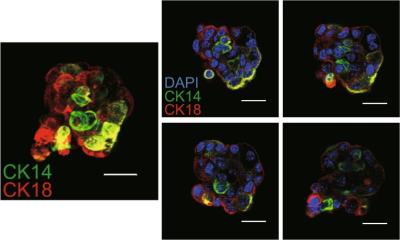
Certain cancer cells evade chemotherapy by entering a dormant cell state. Such cancer cells can persist undetected for several months or even years before they start to proliferate again to give rise to tumor relapse. Although cytotoxic agents are less effective against nondividing cells, drug tolerant persister cells must come up with additional protective measures to cope with the toxic effects of chemotherapy. Researchers led by Gergely Szakács at MedUni Vienna's Center for Cancer Research found that this partially happens through the activation of a protein called P-glycoprotein (P-gp), which helps to clean cells from secondary damage inflicted by chemotherapy.
"P-gp has been well-known as a protein that can export chemotherapeutic drugs from the cells, but its role in protecting dormant cancer cells has not been proven. The discovery that P-gp contributes to the removal of toxic lipids from rare surviving cancer cells represents a vulnerability that can be exploited to prevent relapse. The good thing is that there are already drugs that can block this protein, so we were able to test our hypothesis." explains Gergely Szakács, the lead author of the study.
In a mouse model of triple-negative breast cancer, prolonged inhibition of P-gp prior to the onset of resistance with a drug called tariquidar significantly prolonged the survival of mice, indicating that the critical population of drug-tolerant cancer cells can be targeted by blocking P-glycoprotein. These results could mean that patients with triple-negative breast cancer have a better chance of being cured in the future. Researchers are now working to translate these findings into clinical practice to better treat patients.
Source: Medcal University of Vienna
06.10.2023