Image source: Shutterstock/Kateryna Kon
Sponsored • Infection management
New sepsis marker speeds up detection and therapy
Sepsis is the cause of one in five deaths worldwide, killing nearly 11 million people each year, many of them children. It is also a major cause of disability, affecting millions more. To combat the condition, many hospitals have implemented sepsis performance improvement programmes. A meta-analysis of 50 observational studies showed that these programmes are associated with better compliance with sepsis resuscitation and management bundles as well as a reduction in mortality* in patients with sepsis and septic shock.
Report: Dr Jean Patel
Rapid and accurate profiling of infection-causing pathogens remains a significant challenge in modern healthcare. Most hospitals use blood cultures and other microbiological tests to detect sepsis, while blood culture analysis remains the diagnostic gold standard. However, this method is too slow and cumbersome to significantly influence the initial management of patients. In addition, antibiotic resistance – one of the greatest global challenges of modern time – has become worse with the advent of Covid-19 because it increases the challenge for doctors to differentiate patients who need antibiotics from those who don’t. It is estimated that 72% of Covid-19 patients receive antibiotics when only 8% of patients have co-infection.
Time is of the essence
Blood culture is the most common laboratory method used to identify pathogens responsible for an infection. Cultures obtained within three hours and other diagnostic tools such as PCT and lactate can help identify the risk for sepsis. However, physicians, especially in emergency departments, cannot wait for the results of a microbial culture before pursuing treatment for a potentially septic patient. In fact, delaying intervention is known to increase mortality.
Laboratorians recognise that shortening the time at which pathogens are identified will result in improved patient outcomes in cases of sepsis. Over the last decade, MALDI-TOF (matrix-assisted laser desorption ionisation time-of-flight) mass spectrometry has emerged as an important tool in the quest to speed up microorganism identification. Whereas traditional biochemical microbial identification methods may require days to complete, MALDI-TOF mass spectrometry can provide answers in minutes. These results, integrated with an Antibiotic Stewardship Programme, significantly improve time to optimal therapy while decreasing the length of stay and total costs. A rapid identification combined with accurate antimicrobial susceptibility testing ensures patients get the right antibiotic to treat a life-threatening infection.
A new sepsis marker
In addition to diagnostic tools such as blood culture, PCT and lactate, monocyte distribution width (MDW), a novel sepsis biomarker, is emerging as a valuable resource enabling physicians to make decisions regarding their patients who may be at risk for severe infection.
New analysis from a study confirms that abnormal MDW at presentation consistently increased sepsis probability. Used early in emergency department patients, MDW enhances the odds of early sepsis detection approximately 6-fold utilising Sepsis-2 and ~4-fold based on Sepsis-3 criteria.1
The FDA-cleared MDW in-vitro diagnostic (IVD) parameter is intended for use with adult patients presenting to the emergency department. A complete blood count (CBC) with differential has been ordered to aid in the early detection of patients with or developing sepsis. Together with other laboratory findings and clinical assessments, it provides a qualitative assessment of sepsis from whole blood venous samples. Moreover, the results are automatically available as part of CBC-Diff results for adult patients entering the emergency department with no impact on laboratory or emergency department workflow and no additional tests to order.
* OR 0.66; 95% CI 0.61–0.72
Profile:

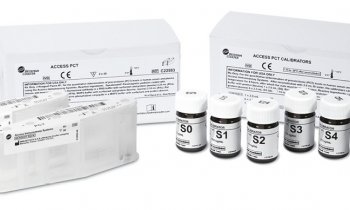
Image source: Beckman Coulter
Dr Jean Patel currently serves as the principal scientist, scientific affairs, at Beckman Coulter. Prior to her role at the company, Patel served as the science team lead, antibiotic resistance coordination and strategy unit, at the Centers for Disease Control (CDC), where she led implementation of its Antibiotic Resistance Laboratory Network and the CDC and FDA Antibiotic Resistance Isolate Bank. Patel has served as chair and vice chair of the Clinical and Laboratory Standards Institute Subcommittee for Antimicrobial Susceptibility Testing and worked with the World Health Organization (WHO) to develop technical guidance for detecting resistance and strengthening global surveillance of antimicrobial resistance.
Reference:
01.04.2022